The human body is made of trillions of cells and hosts an intriguing microbiome - composed of bacteria, fungi, and viruses. These colonies reside in the human body and are vital for digestion and protection. However, not every strain of bacteria is a friend of humans. What happens when the disease causing or harmful bacteria attack the human body? There is a need to destroy them through the use of “Antibiotics” – a well known and commonly used category of drugs.
Antibiotics & Antibiotic Resistance
Certain types of bacteria cause harm to humans. In nature, antibiotics are usually produced by bacteria and fungi. To tackle bacterial infections, antibiotic treatment is adopted as a general practice. Only bacteria cells die when exposed to antibiotics, whereas human cells remain unaffected. Hence, antibiotics are no short of a miracle in healthcare; they are part of the first-line treatment for infectious diseases, safe invasive surgery, and transplants.
When disease-causing bacterial cells develop the ability to survive in the presence of antibiotics or the infections are complex and most likely impossible to treat due to resistant genes it gives rise to the natural phenomenon called “Antibiotic Resistance”. Antibiotic resistance or Anti-microbial resistance (AMR), as it is sometimes referred to, is a big threat in the treatment regimens and hence a big concern for healthcare practitioners worldwide.
The Cause For Antibiotic Resistance
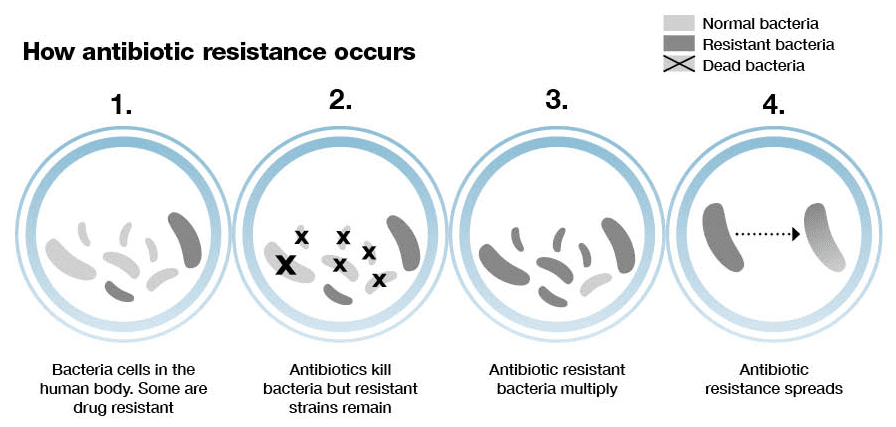
The basic Mechanism:
- A resistant gene is formed due to mutations in the bacterial gene.
- Bacteria can swap genes between cells.
- The occurrence of gene resistance to a particular antibiotic is a rare phenomenon.
- The presence of an antibiotic only kills sensitive bacterial cells.
- The cell's resistant gene proliferates into newer resistant bacterial cells.
- So, each time an antibiotic is used, disease resistance increases within the body.
- The resistant bacterial cells can be easily transmitted.
- Hence, the population eventually becomes resistant to Antibiotics.
History of Antibiotics and Antibiotic Resistance:
- The history of antibiotics can be traced back to ancient times when people used natural substances like honey, garlic, and moldy bread to treat infections.
- The discovery of modern antibiotics is credited to Sir Alexander Fleming, who, in 1928, accidentally discovered penicillin, the first antibiotic. Other antibiotics, such as streptomycin, tetracycline, and erythromycin, were discovered in the following decades, leading to various antibiotics to treat bacterial infections.
In the 1940s, just a few years after the mass production of penicillin began, the first cases of antibiotic-resistant bacteria were reported. Scientists discovered that some bacteria could modify or mutate their genetic material, making them antibiotic-resistant. Over the following decades, more and more antibiotic-resistant strains of bacteria emerged, leading to an increasing number of antibiotic-resistant infections.
The Global Threat
The proliferating Antibiotic resistance across the world will perish the available treatment options. This monstrous consequence can lead to many fatalities and compromised living conditions.
The proliferating Antibiotic resistance across the world will perish the available treatment options. This monstrous consequence can lead to many fatalities and compromised living conditions.
- A study conducted in 2019 by the Indian Council of Medical Research (ICMR) and the National Centre for Disease Control (NCDC) found that more than 70% of bacterial infections in India were resistant to at least one commonly used antibiotic.
- Infections – such as pneumonia, tuberculosis, gonorrhea, and salmonellosis are becoming harder to treat as the antibiotics used to treat them become less effective.
 Identifying The Source: A Basic Necessity
Accurate databases and frequent authorized surveys are crucial to track the production and consumption of antibiotics. It is time to reflect and identify the sources through which people or communities imbibe resistance.
Identifying The Source: A Basic Necessity
Accurate databases and frequent authorized surveys are crucial to track the production and consumption of antibiotics. It is time to reflect and identify the sources through which people or communities imbibe resistance.
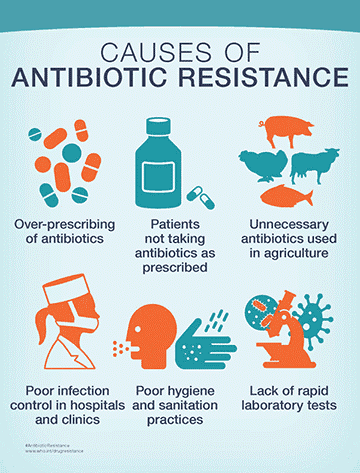
- The antibiotic resistance crisis has been attributed to the overuse and misuse of these medications.
- Antibiotics infiltrated the human food supply chain through many untraceable forms. - Poultry and dairy products.
- Apart from direct sources, every population is affected by this wave of Antibiotic Resistance through indirect means.
- In India, poor sanitation and hygiene have contributed to the rise of antibiotic-resistant infections.
- The widespread availability of antibiotics without prescription has led to their misuse, further exacerbating the problem.
Poultry farming is also one of the prevalent causes of the development of antibiotic resistance in animal protein-consuming communities.
In India, antibiotics are premixed in poultry feed low-dose- (70%) to promote growth and (30%) to combat infections. 11 out of 15 poultry feed constituents used in India are banned by the European Union for agricultural use. A steady stream of sub-therapeutic dose (low-dose) antibiotics is induced during the fattening period in poultry farms to increase livestock weight. This exploitation of Antibiotics in intensive poultry farming and agriculture is prevalent worldwide.
To address this issue, awareness, and accountability are essential. Healthcare professionals, policymakers, the public, and the pharmaceutical industry all have a role in ensuring the appropriate use of antibiotics and preventing the emergence and spread of Antibiotic Resistance.
In India, antibiotics are premixed in poultry feed low-dose- (70%) to promote growth and (30%) to combat infections. 11 out of 15 poultry feed constituents used in India are banned by the European Union for agricultural use. A steady stream of sub-therapeutic dose (low-dose) antibiotics is induced during the fattening period in poultry farms to increase livestock weight. This exploitation of Antibiotics in intensive poultry farming and agriculture is prevalent worldwide.
To address this issue, awareness, and accountability are essential. Healthcare professionals, policymakers, the public, and the pharmaceutical industry all have a role in ensuring the appropriate use of antibiotics and preventing the emergence and spread of Antibiotic Resistance.
National Action Plan To Tackle AMR
World Health Assembly initiated the Global Action Plan on Anti-Microbial Resistance (AMR) in 2015. The action was collaborating with World Health Organization, Food and Agricultural Organization, and World Organization for Animal Health. Union Ministry of Health and Family Welfare released National Action Plan for AMR in April 2017. The Objectives of the National Action Plan are to promote funding for AMR research, provide an authentic database through surveillance, and promulgate awareness of the prevention and control of AMR.
World Health Assembly initiated the Global Action Plan on Anti-Microbial Resistance (AMR) in 2015. The action was collaborating with World Health Organization, Food and Agricultural Organization, and World Organization for Animal Health. Union Ministry of Health and Family Welfare released National Action Plan for AMR in April 2017. The Objectives of the National Action Plan are to promote funding for AMR research, provide an authentic database through surveillance, and promulgate awareness of the prevention and control of AMR.
- Nationwide surveillance and monitoring system must be established to track the production and consumption of Antibiotics all over India. This tracking system would monitor the entire supply chain of Antibiotic use and resistance.
- Policymaking, systematic survey analysis, and information generation on Antimicrobial Resistance are massive resources for Research and Development.
- Curtail the use of Antibiotics in Poultry farming, either by cost increment of Antibiotics or providing awareness on alternate sources.
- Organize training and education programs for farmers, veterinarians, pharmacists, poultry shed supervisors, owners, and consumers, on the safe use of Antibiotics.
- Promote the benefits of proper sanitation measures in farms and highlight the harm of antibiotic use in livestock.
- Ensure licensed antibiotics reach registered users through registered distributors or stockists of veterinary medicines.
- Evidence-based selection of antimicrobials and responsible utilization are possible with technical guidelines and regular clinical audits.
- Phase out the sub-therapeutic use of antibiotics in premixed feeds to promote poultry growth. - this intervention should be monitored and gradual in pace.
Responsibilities At An Individual Level:
While government, policies and healthcare practitioners work together to fight this problem of AMR for better treatment outcome of patients, it is the responsibility of every individual in the globe to understand this menace and follow certain basics to prevent AMR. Few are listed below:
While government, policies and healthcare practitioners work together to fight this problem of AMR for better treatment outcome of patients, it is the responsibility of every individual in the globe to understand this menace and follow certain basics to prevent AMR. Few are listed below:
- Every individual must understand the consequences of the irrational use of Antibiotics.
- Every individual must understand and follow standard hygiene practices.
- Unprescribed and OTC antibiotics must be avoided by every patient.
- The use of antibiotics for viral infections like the common cold is a significant and completely avoidable source of antibiotic resistance.
- Hygiene and good cooking habits must be promoted.
In conclusion, Antibiotic Resistance is a serious threat to global health that requires a concerted effort from all stakeholders. By promoting awareness and accountability, we can prevent the emergence and spread of Antibiotic resistance and ensure that antibiotics remain effective in treating infectious diseases. As Pharmacists or professionals in the healthcare industry, it is a prime responsibility to create awareness and sensitize the community on the perils of AMR and also the prudent use of antibiotics.
Reading Sources:
- The antibiotic resistance crisis: part 1: causes and threats. P T. 2015 Apr;40(4):277-83.
- Antimicrobial resistance: a global, multifaceted phenomenon. Pathog Glob Health. 2015;109(7):309-18.
- Correction: Hand hygiene improvement of individual healthcare workers: results of the multicentre PROHIBIT study. Antimicrob Resist Infect Control 12, 13 (2023).

